
Chapter 3 - Medical & Surgical Treatment Options
Medical & Surgical Treatment Options at Low Vision Optometry of Central Pennsylvania
At present, medical/surgical treatment options for macular degeneration are limited and no treatment is available to actually “cure” the condition or restore the vision loss. Before exploring the current options and current research, let’s first understand what the macula is. This shall be done using some of your imaginative skills:
Imagine The Macula
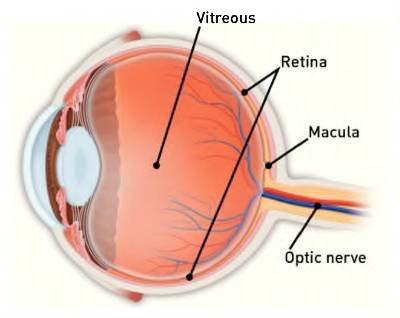 Imagine the room you are sitting in is a great big eyeball and you are sitting in the center of it. If you can face a window that would be the cornea. It’s the clear front structure allowing light into the eye. Behind the cornea is the Iris, the colored portion of your eyes. The black pupil in the center of the iris is actually a hole for light to pass through. Behind the pupil and iris is the crystalline lens. If that clear lens becomes cloudy, it is called a cataract. (The cloudy lens can be replaced with an implant if it is impairing vision). Now look at the ceiling, floor, back and side walls. Imagine those surfaces are covered with wallpaper. The wallpaper represents the retina.
Imagine the room you are sitting in is a great big eyeball and you are sitting in the center of it. If you can face a window that would be the cornea. It’s the clear front structure allowing light into the eye. Behind the cornea is the Iris, the colored portion of your eyes. The black pupil in the center of the iris is actually a hole for light to pass through. Behind the pupil and iris is the crystalline lens. If that clear lens becomes cloudy, it is called a cataract. (The cloudy lens can be replaced with an implant if it is impairing vision). Now look at the ceiling, floor, back and side walls. Imagine those surfaces are covered with wallpaper. The wallpaper represents the retina.
The retina is very thin, comprised of 10 layers and wallpapered to the inside wall of the eye. The layer referred to as rods and cones transform light into electrical impulses that travel down the optic nerve to the brain. In the center of the back wall, about the size of wall clock, If one were there, is an area that is thinner than the rest of the retina and has millions of cone cells packed tightly together. That’s the macula. There are no rods in the macula. Rods are for peripheral vision. Cones are for detail and color (central vision). Vision is sharpest at the macula because those cones are packed so tightly together.
Behind the macula is a network of capillaries- the macula has its own blood supply. That’s why macular degeneration never causes total blindness. The peripheral retina is never affected in macular degeneration; therefore there will always be peripheral (or side) vision.
There are two types of macular degeneration: Wet and Dry.
 1- Dry Macular Degeneration
1- Dry Macular Degeneration
What Take Place
The cells die. There really isn’t anything else to it. The cells die. Why? The major risk factors are age, sunlight, smoking, poor nutrition and genetics.
Dry Macular Degeneration Treatment
There is none. The cones can’t be replaced, can’t regenerate, and can’t be fixed. The only “good” news is that there is usually less vision loss with dry macular degeneration. However, the retina should be monitored and prevention methods taken to avoid progression to the wet type.
2- Wet Macular Degeneration
What Takes Place
The blood vessels behind the macula leak blood or fluid destroying the cone cells. There are numerous treatments available, all designed to stop the leak and prevent further leaks.
Wet Macular Degeneration Treatment
Laser Surgery was one of the first treatments for wet macular degeneration. It sealed the leaky vessels but caused tremendous damage to surrounding cone cells. It is a rarely used procedure at this point.
Visudyne is another earlier treatment option using a pharmaceutical agent injected into the bloodstream. The drug is activated as it passes through the retinal blood vessels by using a low energy laser beam. The Visudyne is activated by the laser which produces a chemical reaction to seal the leak. It is also rarely used at this time.
Avastin/Lucentis/Eyelea are pharmaceutical agents injected into the eye to inhibit proteins called “vascular endothelial growth factor (VEGF)” which stimulate the growth of new, abnormal blood vessels. These abnormal vessels are fragile and leak rather easily. This is the most current treatment option.
” It is unfortunate that none of these treatments will bring back lost vision. None of these treatments are a cure. There are other forms of treatment being researched, two of those being the use of stem cells and electronic chip implants. These are purely investigational at this time and are not considered established medical treatments.”
Recently, there were reports of three individuals who sought stem cell therapy. Stem cells were injected into the eyes. Unfortunately, not only did they fail to help, they caused total blindness in a number of eyes.
With macular degeneration, vision loss occurs when the layer of cells at the back of the retina, the retinal pigment epithelium (RPE) becomes damaged. Stem cell research gives us hope that, someday, doctors will have the ability to regrow the damaged RPE cells.
Electronic Chip Implants are also experimental and are being used for conditions that affect the peripheral (or side) vision like retinitis pigmentosa. They are allowing totally blind people to have light perception. They are not useful for central vision loss at this time.
Prevention / Limiting Vision Loss
 Protect Yourself From UV A&B Lights
Protect Yourself From UV A&B Lights
We know that UV light from the sun is absorbed by the retina and causes damage to the cells. The damage is cumulative over your lifespan. Therefore, it is essential to block all UV A and UV B rays from entering your eyes. Never be in the sun without 100% UV A & B protection.
 If You Smoke, You Should Stop
If You Smoke, You Should Stop
Smoking is a major cause of macular degeneration. Obviously, if you smoke, you should stop. We know that the cone cells require substantial amounts of oxygen and nutrition to keep functioning. The capillaries behind the macula are the main source of these life-supporting molecules. Smoking reduces the amount of oxygen and nutrients in each red blood cell that travels through the capillaries to the macula.
 Changing Your Diet Could Also Help
Changing Your Diet Could Also Help
Adding nutritional supplements and/or changing your diet could also help prevent the onset on MD and has been known to benefit those already diagnosed with macular degeneration. An entire chapter is devoted to nutritional information.
“Unfortunately, we don’t have very good treatments for macular degeneration at this point. However, there are numerous studies now underway to develop new treatments and methods of prevention. Patients must continually check with their eye physician on new possibilities for treatment.”
David Gwynn, MD
Saddleback Eye Medical Associates, Mission Viejo, CA.
